The human jaw is a very important facial feature that can profoundly impact a person’s health and appearance. These bones and muscles work together to enable us to chew, speak, and breathe better. When these components are not working correctly, it can lead to many problems.
Millions of Americans suffer from some form of jaw dysfunction, and many of them require surgery to correct the issue. It is understandable that people have fear or anxiety about correcting these problems. Therefore they do not seek medical consultation and continue to suffer from jaw problems that could be fixed.
At Foley and Le Oral Surgery, we can help assess and correct various jaw problems. Whether your issues are cosmetic, functional or both, we will work with you to create a treatment plan that meets your needs. If you need a consultation and you’re looking for a jaw or oral surgeon in Boulder, CO, Louisville, CO, Lafayette, CO, Broomfield, CO, or Longmont, CO, please come in or call (303) 444-2255 to schedule an appointment. We are located at 1420 28th Street, Suite 100, Boulder, CO.
What Is Jaw (Orthognathic) Surgery?
Jaw surgery is also called orthognathic surgery. It is performed by oral and maxillofacial surgeons, doctors who specialize in correcting irregularities of the face, mouth, and jaws. Orthognathic surgery treats conditions that limit your jaw’s ability to work properly. These conditions often affect your facial appearance and the alignment of your teeth.
Jaw surgery is used to correct jaw bone problems present at birth, problems that develop later in life, or problems caused by an injury. Many people who need jaw surgery have jaws that are out of alignment. As a result, they may have difficulty biting, chewing, and swallowing food.
Jaw surgery may be recommended for:
- An improper bite due to crowded or missing teeth
- Facial trauma
- Jawbone deformities present at birth
- Obstructive sleep apnea
- Difficulty in chewing, biting, or swallowing
- Speech problems
- Chronic pain of the TMJ (jaw joint)
- Open bite
- Protruding jaw
- Receding chin
- Inability to make the lips meet without straining
- Breathing problems
- Excessive wear of the teeth
- Unbalanced facial appearance from the front or side
Why Correct a Bite Problem?
If you have a problem with your bite, it is important to seek treatment because it can lead to several other problems. Some patients may not think that bite disorders are a big deal, but they can lead to many future issues, including tooth loss.
Bite disturbances can cause:
- Chronic pain in the jaw joints (TMJ)
- Headaches
- Tooth wear and fracture
- Clicking, popping, or grinding noises in the jaw joint (TMJ)
- Ear pain
- Muscle fatigue
Types of Jaw Surgery
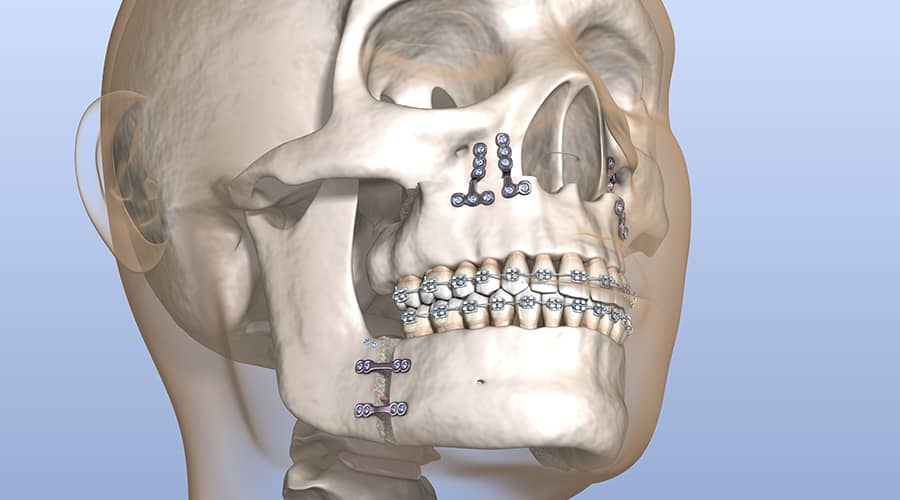
When performing your surgical procedure, the surgeon will make changes to the bones of your upper jaw, lower jaw, or both and realign them into a more functional and aesthetic position.
There are four types of jaw surgery:
- Maxillary osteotomy surgery: This type of surgery corrects problems with the upper jaw. It is also called LeFort osteotomy.
- Mandibular osteotomy surgery: This type of surgery corrects problems with the lower jaw. It is also called sagittal split ramus osteotomy or bilateral sagittal split osteotomy (BSSO).
- Combined Maxillary and Mandibular Surgery: This type of surgery corrects problems with both the upper and lower jaws.
- Chin Surgery: This type of surgery correct the position of the chin and is done in combination with the mandibular osteotomy surgery. It is also called a geniplasty.
Orthognathic Surgery Consultation
The consultation is a very important part of the process. You will meet with one of our surgeons during your consultation to discuss your concerns and learn more about your treatment options. When considering jaw surgery, it’s vital to know exactly what the procedure will entail and what will be required of you. You might have an idea of what you want the outcome to look like. But it’s also important to be realistic about the results.
The principal goal of jaw surgery is to ensure that the teeth function in an optimal way following surgery by improving jaw alignment. Jaw surgery is not done principally for esthetic concerns, however, jaw surgery helps to achieve skeletal balance between the upper and lower jaw and therefore frequently results in a positive esthetic change.
Jaw surgery is a big decision, and we want you to feel confident and comfortable with your choice. We encourage you to ask lots of questions during your consultation so that you have all the information you need to make an informed decision.
During your consultation, your surgeon will:
- Conduct a thorough medical history and oral and facial examination
- Assess how well you chew, bite and swallow
- Evaluate the way your teeth fit when you bite together
- Take X-rays of your mouth and face
Virtual Surgical Planning (VSP)
Dr. Foley and Dr. Le utilize virtual surgical planning (VSP) to help plan and perform the jaw surgery. VSP is used to create customized surgical cutting guides, bone plates and occlusal splints which is used during the procedure. VSP will show you exactly how your surgery will be performed using modern computer technology and three-dimensional models. They will show you how they will improve your bite and show you images of the expected outcome. Their goal is to help you understand the process of the surgery and the treatment that is being prescribed specifically for you.
Pre and Post-Surgical Orthodontic Treatment
The treatment of most bite abnormalities (malocclusion) is usually accomplished by orthodontics alone. Surgery is necessary when an abnormality in the jaws’ position, shape, or size prevents bite correction by orthodontic tooth movement alone.
Surgery may be desirable in situations where the bite problem could be improved by orthodontics alone, but the results would be unstable or unsatisfactory, functionally and/or aesthetically. As abnormalities of tooth position and jaw deformity usually co-exist, it is almost always necessary to combine surgery and orthodontics to achieve an acceptable treatment result.
It is typically necessary to align the teeth orthodontically before corrective jaw surgery. This may require braces to be worn from a few months to a year or more before surgery. During the pre-surgical orthodontic phase, dental impressions of your teeth will be obtained to determine when your teeth are in the proper position to undergo surgery. These dental impressions will be obtained by the orthodontist or your surgeon. In either case, your orthodontist and oral surgeon will consult regarding the models, and a decision will be made based on the status of the pre-surgical orthodontic preparation.
Your orthodontist will begin the finishing phase of orthodontic treatment approximately 6-8 weeks after surgery. Two to twelve months may be required to complete the orthodontic treatment. The last few months of orthodontic treatment consist of the final adjustment of tooth positions, after which the orthodontic appliances will be removed. The orthodontist will place retainers that should be faithfully worn indefinitely to make sure the teeth stay in the desired position.
The Surgery
Jaw surgery is performed under general anesthesia, which means you will be asleep during the procedure. The surgery time will depend on many factors but may take longer if you are having multiple procedures or if there are complications.
Corrective jaw surgery requires a brief hospital stay for 1-2 nights. In some cases, lower jaw operations may be done on an outpatient basis, although most patients will remain in the hospital and be discharged on the first day following surgery.
It is important to follow up with your surgeon for regular post-operative visits. During these appointments, your surgeon will evaluate your progress and make necessary adjustments to ensure that you are healing properly. Following surgery, the first follow-up visit will be one week after surgery, with additional visits approximately every two weeks until the surgery has completely healed at 6-8 weeks.
What To Expect After Jaw Surgery
Scars: Corrective jaw surgery is generally performed inside the mouth; therefore, no external scars are produced. Occasionally, a very small (less than ½ inch) neck incision is required to place jaw screws to stabilize bone fragments. These incisions will leave a scar that generally is cosmetically acceptable. These incisions are made on less than 10% of patients.
Irritation of the corners of the mouth always occurs with corrective jaw surgery. This appears as an abrasion and may form a scab. Noticeable scarring from this irritation is uncommon.
Jaw fixation (immobilization): Occasionally, your jaws may be wired closed in a predetermined position at the time of surgery to allow healing to proceed satisfactorily. The period of jaw immobilization is generally 1-6 weeks. During this time, you will only be able to consume liquids. All medications that are prescribed will be in liquid form. Any regular medications that must be taken in pill form may be crushed and taken with the liquid of your choice.
After the wires holding your mouth closed are removed, you will be shown how to wear orthodontic elastics. Elastics will be worn approximately 23 hours/day until you are 6-8 weeks out from surgery. You can remove the elastics at mealtime.
If you have had lower jaw surgery, your lower jaw will be temporarily stiff, and your ability to open your mouth will be limited. Jaw opening exercises will be started after surgery. It usually takes several weeks of active exercises to regain most of the jaw opening.
Speech: Clear speech is more difficult when the jaw is wired closed. Patients differ in their ability to speak following jaw surgery. Typically patients can be understood, although telephone conversations may be slightly more difficult.
After surgery, you should express your needs by talking as much as possible, not by writing notes. During your surgery, an acrylic wafer(s) that was fabricated before your surgery will be placed in your mouth to ensure your bite is properly aligned. The wafer(s) will make speech more difficult. They are generally removed 6 weeks after surgery.
Diet: When you are wired closed, your diet will consist only of liquids. Dietary instructions and samples of high-calorie/high protein liquid diet supplements will be given to you before your surgery. For the first 24 hours after surgery, you will be restricted to clear liquids (tea, apple juice, Sprite, etc.). After the first 24 hours, you will be encouraged to drink a high-calorie, high-protein liquid diet.
After you begin using elastics, your diet will be advanced to very soft foods that do not require chewing. You should not chew until at least six weeks after surgery. You should be able to resume an unrestricted diet by eight weeks after surgery. You can expect to lose 5-10 pounds during the first two weeks; after this time, you should be able to maintain your weight.
Loss of appetite after surgery is common and, apart from the jaws being wired closed, will contribute to early weight loss. Usually, by one week after surgery, your appetite will improve to the degree that most patients can maintain or possibly gain weight.
It is very important to take in an adequate volume of liquids during the first 5-7 days after surgery. Dehydration can and must be prevented by consuming at least 1-2 liters (the volume of ¼ to ½ a gallon of milk) of liquid each day.
Swelling and bruising: Facial swelling should be expected after corrective jaw surgery. Bruising is less common but does still occur on a relatively frequent basis. The amount of swelling varies depending on an individual patient’s response to surgery and the type of surgery performed. Maximum swelling is generally reached within 72 hours of surgery. Most swelling can be expected to subside within 1-2 weeks. Some mild residual swelling may persist for several months.
Ice packs will be used immediately following surgery, and patients are routinely given special medication through an I.V before, during, and after surgery to reduce the tendency to swell. You should keep your head elevated above the level of your heart for at least the first three nights after surgery. You can do this by sleeping on at least two pillows or in a recliner chair.
Occasionally drain tube(s) will be placed into a wound to reduce the accumulation of blood in the tissues. Such a drain tube(s) will exit the wound through the skin below your chin. Most drains can be removed in the hospital the day after surgery. Despite these efforts, some patients will have a great amount of swelling, especially involving the lips.
Pain: Most patients have only moderate pain after corrective jaw surgery. Low-grade “discomfort” is common and responds well to pain medication. A few patients will describe severe pain, likely due to differences in individuals’ pain tolerance. A prescription for liquid pain medication will be provided after surgery.
Occasionally, patients will complain of jaw joint (TMJ) pain after surgery. This is more likely to occur if you had surgery to advance the lower jaw. This pain usually subsides but, in rare circumstances, may persist for weeks or months after surgery.
Recovery
Recovery times vary from person to person, but it generally takes about six to eight weeks for the bones to heal after jaw surgery. During this time, you will likely experience discomfort and need to stick to a soft food diet as your jaws heal. It’s important to take things easy during your recovery and not push yourself too hard.
- Most patients take two to four weeks off from work or school to recover, but this will depend on your surgery and how well you are healing.
- You should avoid any strenuous activity during your recovery so that you don’t put too much strain on your healing bones and avoid contact sports for 12 weeks.
- Do not smoke for a minimum of 8 weeks during your recovery, as this can impede healing and result in the loss of teeth and jaw bone segments.
- Oral care is very important during your recovery. Be sure to brush and floss twice daily followed by the use of the prescribed medicated mouth rinse.
(Note: For detailed instructions before and after jaw surgery, refer to the Jaw Surgery Surgical Instructions.)
Risks of Jaw Surgery
As with any surgery, there are risks associated with jaw surgery.
These include:
- Anesthesia risks. All surgeries that require anesthesia have a small risk of complications. This is why it is important to have a thorough preoperative evaluation by your doctor.
- Infection. There is a small risk of infection with any surgery. This risk can be reduced by taking antibiotics as prescribed by your surgeon. In rare cases, a sinus infection will result from upper jaw surgery. It is possible for a patient to develop a serious infection that will require hospitalization for management with I.V antibiotics and possibly surgical drainage.
- Extraordinary blood loss/blood transfusion. A blood transfusion may be necessary for patients who undergo surgical repositioning of the upper jaw or both jaws. Because of this, you will be given the option to donate 1-2 units of your own blood before surgery. Extra precaution is taken during the procedure to ensure minimal blood loss; however, extraordinary, life-threatening bleeding can occur. If this happens, blood in excess of what was pre-donated might have to be used. Though blood-banked blood is carefully screened for infectious diseases, no blood is entirely safe for transfusion. If you are opposed to a blood transfusion, you must discuss this with your surgeon before surgery.
- Relapse. Relapse is the tendency for a tooth that has been moved by orthodontics or a jaw that has been moved with surgery to return to the pre-treatment position. It is common for there to be some relapse in all cases of orthodontic treatment and corrective jaw surgery. With the technology and knowledge available today, your surgeon and orthodontist can diagnose most problems and suggest proper treatment. Relapse is more likely in situations where an open bite and/or a short lower jaw is being corrected in the setting of jaw joint (TMJ) disease.
We aim to do all we can to ensure that repeat surgery is not necessary. However, every patient is different, and every case is different. From time to time, we will see exceptions to patients’ usual response to treatment.
It is desirable not to have to re-operate on a patient as a result of unacceptable relapse. However, in the case of significant relapse, repeat corrective jaw surgery may be necessary.
- Temporomandibular joint (TMJ) problems. Corrective jaw surgery is rarely done to improve jaw joint (TMJ) symptoms or function. Pre-existing TMJ symptoms may remain the same, improve, or worsen with corrective jaw surgery. Some patients with pre-existing TMJ disease will experience new symptoms at some point after corrective jaw surgery. Fortunately, this is not a common occurrence. Corrective jaw surgery may speed up pre-existing TMJ deterioration for reasons not completely understood. This may occur without pain or other symptoms. Patients who have had corrective surgery for a severe open bite or a short lower jaw may experience joint deterioration that may cause exceptional relapse. TMJ deterioration rarely occurs in a patient who does not present for surgery with pre-existing joint deterioration. Even if symptom-free, patients with pre-existing TMJ disease should clearly understand this potential problem.
You can reduce your risk of complications by following your surgeon’s instructions and attending all follow-up appointments.
Jaw and Oral Surgery in Boulder, CO
Understanding your jaw issues and personal goals is critical to choosing the right treatment for you. We will create a personalized treatment plan for your unique situation. Jaw health is essential to overall health and function, so don’t wait to seek treatment. If you need jaw or oral surgery in Boulder, CO, Longmont, CO, Broomfield, CO, Lafayette, CO, or Louisville, CO, call (303) 444-2255 to schedule a consultation today.
Call UsFrequently Asked Questions
Jaw surgery is a big decision and not one to be made lightly. However, it can greatly improve your quality of life by improving your eating, speaking, and breathing abilities.
Jaw surgery is a major surgery and therefore is associated with discomfort. However, your surgeon will take steps to minimize your pain and help you through your recovery.
You will be able to talk after jaw surgery, but your speech may be slightly slurred or more challenging. This is usually temporary and will improve as you recover and the surgical occlusal splints are removed.
Jaw surgery may be recommended if you have severe crowding of the teeth or an overbite, underbite, or open bite (front teeth do not touch) that cannot be corrected with braces alone.
You should not fly for at least six weeks after jaw surgery. This is to prevent any complications from changes in cabin pressure. Please speak to your surgeon if you have any questions as every situation is different.
Jaw surgery usually results in some changes to the shape of your face, but this is usually subtle. You will still look like yourself, just with a more balanced appearance. Jaw surgery is not performed for esthetic purposes. It is done to correct functional chewing and breathing problems. However, frequently the changes to your face following jaw surgery will be viewed as a positive esthetic change.